
The average healthcare worker isn’t prepared to fully comprehend all the touch points of care, let alone the government perspective on reimbursement that is tied to performance metrics. Regulatory mandates, whole person care, facility quality measure selection, provider engagement, accountability and transparency and measuring outcomes can easily be overwhelming. Often, you might not be sure how to formulate specific patient-centered navigation or address questions that allow the patient to better understand what to expect.
Where to start
Key points for you to consider:
- Data infrastructure:
Governments need robust data systems to accurately capture patient outcomes and quality measures, which can be challenging due to varying data standards across healthcare providers and systems.
- Risk adjustment:
To ensure fair comparisons between providers, adjustments are made based on patient demographics and health status, preventing penalizing providers treating complex patient populations.
- Quality measure selection:
Choosing relevant and meaningful quality measures is critical to drive desired improvements in patient care and should involve stakeholder input.
- Provider engagement:
Effective communication and education are vital to ensure providers understand the value-based care model and actively participate in quality improvement initiatives.
- Financial incentives:
The structure of financial incentives, including potential upside and downside risk, can significantly impact provider behavior and adoption of value-based care practices.
- Accountability and transparency:
Public reporting of provider performance data can encourage competition and patient choice while also raising concerns about potential disparities and stigma.
- Impact on vulnerable populations:
Governments need to consider how value-based care models might affect access to quality care for underserved communities and address potential disparities.
From a government perspective on reimbursement tied to performance metrics and value-based care, one should also understand the complexities of designing and implementing these programs, including: data collection and analysis, risk adjustment mechanisms to account for patient demographics, provider engagement strategies, quality measure development, and the potential for disparities in access to quality care across different populations; essentially, ensuring that the system incentivizes high-quality care while mitigating potential biases and unintended consequences.
Example government initiatives, * data is located online (see note below):
- Medicare’s Hospital Value-Based Purchasing (VBP) Program:
Penalizes hospitals with poor performance on quality measures and rewards those exceeding benchmarks.
- Hospital Readmission Reduction Program (HRRP):
Imposes penalties on hospitals with high readmission rates for certain conditions.
- MACRA (Medicare Access and CHIP Reauthorization Act):
*Note: Works of the U.S. Government are in the public domain, and you don’t need permission to reuse them, but an attribution to the agency as the source is appreciated. Your materials, however, shouldn’t give the false impression that the government’s endorsing your commercial products or services. See 42 U.S.C 1320b-10.
This information below is separated into sections that speak to regulatory mandates past, present and what may be underway for the future. We provide the links to easily find government initiatives. You can choose what you want to know, how you want the information delivered, or what we might have missed, so we can create your to-do list to educate your staff.
This level of membership has many moving parts, changes, and perspectives along with multiple levels of complexity. This level of Facility level membership gives you a comprehensive look aligned with different levels within your organization. We have organized this level of membership using a “top to bottom” approach.
- For those just starting, “Level One” we provide an easy-to-read Yale Law School Legal review of what and why hospitals are tasked with improving the health of the communities they serve. Understanding accountabilities, responsibilities, and community health, as it correlates with the Affordable Care Act, and the American Hospital Association helps to educate and explain important topics such as the Value Initiative
- Next, we speak to the Federal Agency for Healthcare Research and Quality (AHRQ) who is tasked to provide the knowledge, tools, and data needed to improve America’s healthcare systems
- Facilities and Organizations are tasked with understanding multiple “datasets” of information, we provide workflows and report categories that save time in looking for the data you need by designing custom templates.
- If you like numbers and want to find areas to increase bottom-line indicators, we have organized these metrics as well
- Next are a listing of various types of care facilities, understanding percentile rank and how you compare with others is organized by facility, state and national performance. We can teach you how to track performance over time too! Just ask!
- Outpatient Ambulatory Surgery (OAS), a growing service line, is explained using the same methodology and we’ve included the link to the recent rule published annually on the Federal Register along with links to areas policy experts are debating
- The comprehensive mid-level membership, Clinicians and Providers is included
- The last section is our comprehensive Consumer and Caregiver level membership information
Let’s get started with some simple descriptions, with links that take you to websites that speak to current and, in some instances, the proposed or innovative future state.

The question hospital leaders consider when prioritizing the findings include; what the socio-economic conditions are along with neighborhood and physical environments in which people are born, grow, live, work and age. These are referred to as “Social determinants of health” (SDOH) and address ‘the structural determinants and conditions in which people are born, grow, live, work and age.’” According to a report from the Kaiser Family Foundation, “They include factors like socioeconomic status, education, the physical environment, employment, and social support networks, as well as access to health care.”
Although it may seem impossible for the IRS to “police” compliance, research shows that a meaningful number of hospitals are engaged in serving the most vulnerable and needy populations. Learn more about the Affordable Care Act (ACA). The American Hospital Association (AHA) has multiple tools, resources, and Forums along with the latest news related to the Accountable Health Communities model. They do a nice job with multiple approaches in educating and explaining topics such as the Value Initiative, which speaks to how hospitals are driving value in their communities. The AHA is looking for you to tell your success stories, are you a member?

CMS continues to make major strides in realigning their Research, Statistics, Data & Systems information and our intention is to help you navigate the information and provide some guidance related to report utilization. Datasets and Topics are drawn from the Medicare Care Compare website and directories. For those interested in the math and calculations, we found the most recent Payment Error Rate Measurement (PERM) Manual that was updated May 2020.
The intent of Purposeful Concepts LLC is to keep you up to date, with just a click to the most recent report area. However, as we promise to educate and support your teams, keep these facts in mind:
- As CAHPS data updates, typically on a quarterly basis, the oldest quarter “falls off the listing”
- When you download the data, you can save the “rolling” time periods
- We propose the file name to have a naming convention that aligns with a crosswalk or the actual dates encompassed in the report
- This allows you to compare and watch trends that may align to in-house action plans as it relates to their effectiveness
- How you watch trends in data requires this initial question,
- “what is the story you are wanting to tell
- “who is the audience you are reporting to?”
- Are you wanting to promote a service line
- determine a financial outcome
- address how a patient and family initiative is progressing
As you review the data on the links below, think about how you will calendar a standardized time each quarter to retrieve and save the data you are responsible for.
Data can be sorted and searched by using the filter at the top of each column
To expand the view, look to the right and select Manage Columns, all columns are selected by default.
Deselect the ones you do not want in your report and hit the “Update Columns” button at the bottom.
Sort by; Fiscal Year, Facility ID, Facility Name, Address, City, State, Zip and then by the measure(s)
The report categories we have readily made available for you include:
Hospital Value-Based Purchasing (HVBP) – Person and Community Engagement Domain Scores (HCAHPS) Here you will find a list of hospitals participating in the FY 2021 Hospital VBP Program and their scores for the Person and Community Engagement HCAHPS dimensions. Notice the “last updated” date noted.
Keep in mind not all the reports may have the same date.
Under the Dataset explorer the rows mentioned speak to the number of facilities across the nation participating.
If you were a user of the older version of Hospital Compare, these areas were reported but the user was limited to selecting three facilities, now the dropdown allows for 100 rows per page.
The VBP data is separated by each VBP measure, which we have highlighted the term that was on the prior site for your convenience.
Our hyperlinks will provide the user with the most current CMS posting. There is no set schedule to follow so when you click on a link with a 2022 reference, it can take you to a future time period report as our links provide the most recent update from CMS.
Hospital Value-Based Purchasing (HVBP) – Efficiency Scores
A list of hospitals participating in the FY Hospital VBP Program and their performance ratios and scores for the Efficiency and Cost Reduction Medicare Spending per Beneficiary (MSPB) measure.
Hospital Value-Based Purchasing (HVBP) – Total Performance Score
A list of hospitals participating in the FY Hospital VBP Program and their domain scores and Total Performance Scores.
Hospital Value-Based Purchasing (HVBP) – Clinical Outcomes Domain Scores
A list of hospitals participating in the FY Hospital VBP Program and their performance rates and scores for the Clinical Outcomes measures.
Hospital Value-Based Purchasing (HVBP) – Safety
A list of hospitals participating in the FY Hospital VBP Program and their performance rates and scores for the Safety measures.
Hospital Value-Based Purchasing (HVBP) – Person and Community Engagement Domain Scores (HCAHPS) Are a list of hospitals participating in the FY 2022 Hospital VBP Program and their scores for the Person and Community Engagement HCAHPS dimensions.
The next set of links relate to four tables that typically relate to finance, again watch the dates:
Table 1: FY Net Change in Base Operating DRG Payment Amount
Net Change in Base Operating DRG Payment Amount shows number of hospitals for specified ranges of value-based incentive payment amounts after subtracting the amounts after subtracting the amount by which their Medicare payments per discharge were reduced.
Table 2: FY Distribution of Net Change in Base Operating DRG Payment Amount
Distribution of Net Change in Base Operating DRG Payment Amount shows the distribution of hospitals value-based incentive payment amounts after subtracting the amount of the applicable percent reduction from their Medicare payments
Table 3: FY Percent Change in Medicare Payments
Percent Change in Medicare Payments displays how hospitals’ Medicare payments changed as a result of the Hospital VBP Program in percentage terms.
Look for the update date; as you begin to look at data you may notice the progression occurs quarterly, but sometimes it may seem like there is a four month release due to an actual day of posting that makes in fall into the following month (December, April)
Table 4: FY Value-Based Incentive Payment Amount
Value-Based Incentive Payment Amount displays the number of hospitals that received value-based incentive payment amounts in ranges of $50,000.

In these examples we have highlighted, by Facility, by State, and by National to provide concepts on different audiences using or viewing the data.
Inpatient Psychiatric Facility Quality Measure Data – by Facility
If your facility is a part of several within a system, by facility allows you compare outcomes or find opportunities to explore and model “best practice” within your own system where one is meeting the requirements or objectives and others are not. This data is necessary on every report where National data is mentioned. To receive the highest reimbursement amount within a pay-for-performance (P4P) methodology, you need to be at or above the National score to earn back withheld performance dollars.
Inpatient Psychiatric Facility Quality Measure Data – by State
When you compare facilities at the state level, and your facilities are meeting the program requirements and others are not, this speaks to your “brand” or is a starting point for a marketing campaign. Often times this concept speaks to service lines or care that is close to home when out-migration data shows patients are seeking care outside of the facility service area.
Inpatient Psychiatric Facility Quality Measure Data – National
In all three of these examples, Psychiatric facilities that are eligible for the Inpatient Psychiatric Facility Quality Reporting (IPFQR) program are required to meet all program requirements, otherwise the Annual Payment Update (APU) reflects the reduction in Medicare payments.

CMS measures metrics through the Outpatient and Ambulatory Surgery Consumer Assessment of Healthcare Providers and Systems (OAS CAHPS) survey for hospital outpatient departments – with this example reporting by Facility which allows the user to sort by state using the filter. If you scroll all the way to the right, you can prepare a report based on specific questions.
This is an excellent way to teach, those patients & families who are participating in process improvements, to use the public tool on their own device while allowing HIPPA compliance.
The other feature of this tool is when high scores are reported around specific measures, the facility phone number is a part of the fields display allowing for possible collaboration.
A list of hospital outpatient department ratings for the (OAS CAHPS) survey data are updated and reported each quarter with data from the most recently completed quarter replacing the oldest quarter of data. The data reporting period is included in the tables.
Ambulatory Surgical Quality Measures – Facility
The link above is a list of ambulatory surgical centers participating in the Ambulatory Surgical Center Quality Reporting (ASCQR) Program and their performance rates. You might want to find the current measures for the CY Payment Determination and program requirements as well as the most recent rule that is published annually on the Federal Register.
As we explore measures, new questions may come to mind related to research, latest insights, and what areas policy experts are debating. The RAND Corporation is an interesting site that speaks to research from different perspectives. We recommend looking at some of the research concepts available there too.
Tell ME About YOU!
Below is an overview of what we offer in our mid-tier membership
the Clinicians and Providers, that you might find of interest.

Welcome to Purposeful Concepts LLC (PC) and our PC User Guide. This guide is updated and expand as care processes, workflows, with built in links to multiple government sites and information related to best practice Measures Under Consideration (MUCs), Pay-for-Performance and Value Based Purchasing along with regulatory compliance mandates and tools to meet specific measures. Our goal is to walk you through various “recipes” for improved outcomes in care, patient experience indicators, navigation of best practice information and custom tools to help you reach your goals. As with any recipe, modifications, scale, and substitutions are always possible.
Becoming a physician is no small feat, and most times in depth education wasn’t embedded in your curriculum. The complex regulatory mandates keep evolving, especially since Telemedicine and Telehealth was thrust into the forefront due to the SARS-CoV-2 Pandemic. Patients and families and their providers, working together, will continue to evolve and patient and family literacy in navigation and their case management brings new challenges. Many find care alternatives in the Quality Payment Program (QPP) and the resource library navigation daunting.
If you are just beginning the journey, you may find regulatory mandates both challenging, time consuming AND ever-changing. It may seem just when you begin to understand the information and workflow, the government has a new policy to align with. With that, now comes the necessity to understand what, why, and how the change will affect the work you and the facility you guide or your private practice will be held accountable or responsible to do. Who is on your team to guide you? What email is linked to the NPI numbers in your practice? What happens when the person responsible for that role moves on? These are just a few questions to consider.
If you have surrendered and become a part of a “system” or lead their “think tank” we offer a plethora of resources to consider with the tools just a click away. Is your compensation correlated with quality and/or patient experience metrics? How will you meet the facilities objectives; if you are the lead for your department or team can you explain why the objective is important?
The good news is, our site saves you precious time with access to resources as well as payroll dollars. Let us know if you need something not mentioned here as we update quarterly or as needed. We have a “Tell Me About You” section below where you can request a need that isn’t in our general PC User Guide layout.
Clinicians and Providers: Looking for a way to understand where to start? The for becoming a member, you have unlimited use of a glossary of terms and other tools to guide you through the transformation of care and complex healthcare information. We help providers to engage with their patients and families to secure the best possible outcomes. Lead your team with best practice healthcare information methods found in our Purposeful Concepts User Guide
Quality Net / HCQIS has a new site, https://qnetconfluence.cms.gov/display/HS/CCSQ+ServiceNow
Are you one of over 1000 User Groups affected by the HCQIS ServiceNow Update? Looking for the Release Information will require you to log in signing in.
CCSQ ServiceNow is the powerful ticketing tool that the CMS Center for Clinical Standards & Quality (CCSQ) community uses for asking questions, reporting something not working right, and requesting something new. When a customer opens a new ticket, the ServiceNow app emails them a reference number and status. To obtain the status of a case, incident, or request, customers can simply reply to a ServiceNow email notification or track an existing ticket on CCSQ Support Central. Opening tickets isn’t all that we do! Did you know that we also modernize IT? Click here to learn more.
We know scheduling time to view a live webinar where you can learn what is underway or navigate the plethora of websites might at times seem impossible. Let us know if there is a specific area that we can incorporate into our Blog area or provide a link through social media.
National Government Services (NGS) just launched a new site for those wanting to expand their experience within Medicare with multiple tools organized in an easy to look up or learn more.
We include the note related to government websites to inform you that our intention is to organize information into a comprehensive methodology for you to efficiently navigate to the topics of your interest and do not use their graphics but link you directly to their evidence.
Note: Works of the U.S. Government are in the public domain and you don’t need permission to reuse them, but an attribution to the agency as the source is appreciated. Your materials, however, shouldn’t give the false impression that the government’s endorsing your commercial products or services. See 42 U.S.C 1320b-10.
Additionally, we’ll let you know what the upcoming subject matters are through our Blog page, social media or push notification direct to your inbox, You choose what you want to know about and how you want the information delivered. If there is something specific, no problem, use our “How Can We Help?” custom request form below, select “other” and use the comments box to notify us. Sometimes we aren’t sure how to ask the specific question, if that’s the case explain what the barrier is to achieve the desired results.
This page is separated into sections that speak to regulatory mandates past, present as well as what may be underway for the future. This level of membership has so many moving parts, changes, and perspectives along with multiple levels of complexity. Let’s get started with some simple descriptions with links that take you to a website that can speak to current and, in some instances, the proposed or an innovative future state.

Most Importantly, understand how the progression from 2011 to current state certainly will change as we move into 2022.
More recently, The Office of the National Coordinator (ONC) for Health Information Technology (IT) released a 10-year vision paper for the state of health IT by 2024. The goal is to achieve interoperability among the various health IT platforms, which in turn would help reduce costs, allow patients more control over their information and decision making, and generally improve patient health.[7]. The 10-year vision paper is a nice 12 page overview, and we highly recommend taking a look especially if you are in private practice, haven’t fully implemented your patient portal, or have a general idea as to what needs to be accomplished by 2024, just a few short years away. If you are ready for a deeper dive, take a look at the Complete Milestones, Call to Action and Commitments found in the 94 page final version of “Connecting Health and Care for the Nation” A Shared Nationwide Interoperability Roadmap.

- understand what questions to ask from a provider perspective
- know what resources are available for developers and vendors
- want to better understand how patients, consumer, or caregiver learn more
The links above are really amazing free resources. The education offered on the provider perspective comes with additional features such as:
- A state innovative model resource center
- Understanding the benefits of a Health Information Exchange (HIE)
- Privacy and Security Laws (HIPPA) information
HIPPA Compliance can be complicated, check out this group that handles all compliance measures for you.
The Affordable Care Act (ACA) is the comprehensive health care reform law enacted in March 2010. The three primary goals relate to
- Making insurance affordable to more people
- Expansion of the Medicaid (state) program (not all states have expanded their program)
- Support innovative care delivery methods designed to lower the costs of general healthcare
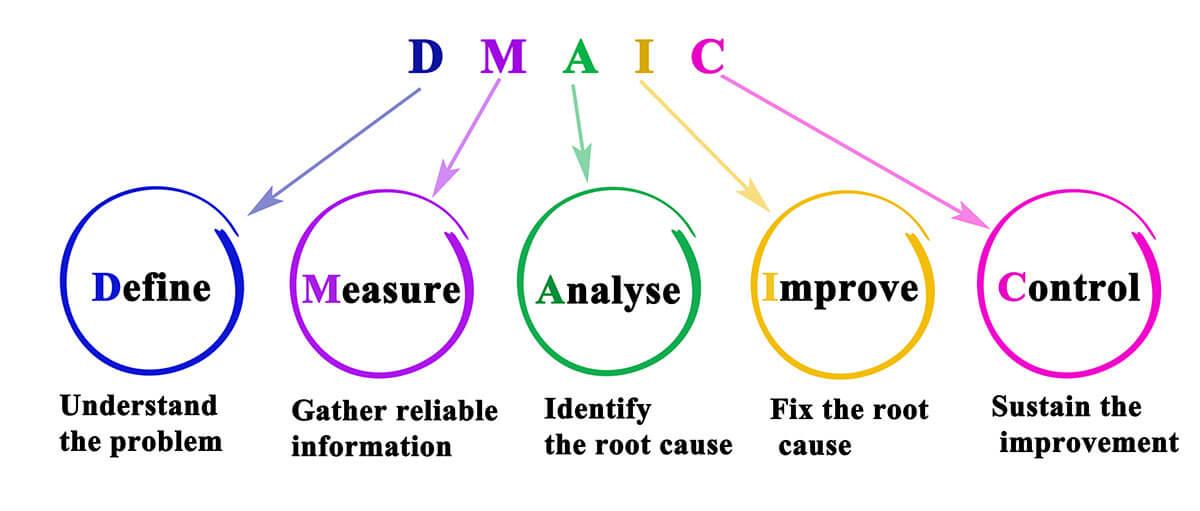
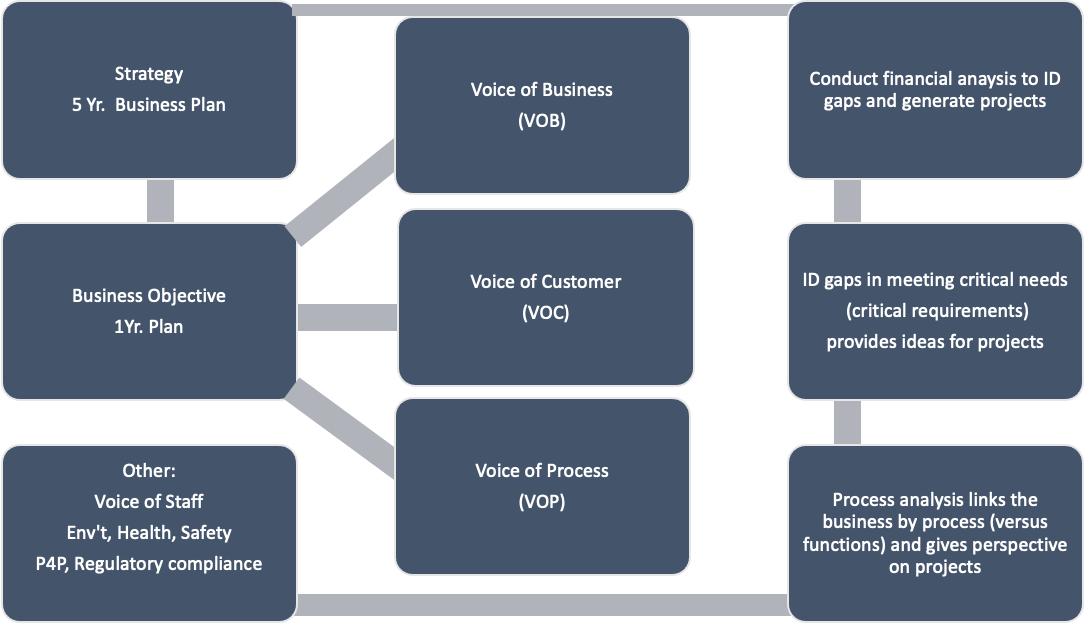
The DMAIC model helps team members, who typically don’t join an improvement project until after the problem has been identified. Target areas (project identification) are usually identified by looking at what’s important to the business (known as the “value levers” that include cost, profit, revenue, customer segments, etc.). Ideas can be gathered from various sources such as customer surveys, process data, marketing information, employee opinions as well as regulatory changes. Simple framework can look something like this:
From responsibilities in:
- communicating
- data transmission
- and necessary fields your vendor would set up,
- knowledge of the E.H.R version (CHPL)
- how your patient portal is integrated
- as well as Promoting Interoperability Programs
Determine if you are up-to-date or need to learn more; below are resources for the following years:
- Certified E.H.R. Technology
- CAHPS The Consumer Assessment of Healthcare Providers & Systems patient survey
- 2020/2021 Program Requirements Medicaid
- Medicare and Medicaid Promoting Interoperability Program Basics
- Electronic Clinical Quality Measures Basics
- FAQs review E.H.R. incentive Program questions and answers by topic
- Data and Program Reports
- Medicaid (state information) eligible professionals
- Registration and Attestation Medicaid (state) User Guide and additional resources
QualityNet (QNET) your one-stop shop for CMS Quality Programs has taken an aggressive approach to modernize and enhance many common technologies as CMS looks to the future of supporting healthcare across the nation. The News area speaks to features and updates such as the one for Electronic Clinical Measures (eCQMs). The NEW public hub for Healthcare Quality Information System (HCQIS) offers news, guidance, and information on QualityNet IT services. Onboarding information for contractors, and The Roles are easily found as are Service and Support Materials.
Data submission and transmission will continue to grow and guide care models. For those of you familiar with the Quality Payment Program (QPP) their tool allows the user to look at a specific measure and activities for each performance category under the traditional MIPS program.
This tool is for planning only and will not submit anything to CMS.
Once you select the Performance Year, the measures (Quality Measures, Promoting Interoperability, Improvement Activities and Cost Measures) and the percentage they made up for the performance period, are easily sorted and navigated.
For a new user, the QNET Resource Library is VERY valuable as is the Webinar Library.
Your vendors should be available to assist with configuration and guidance.
To give you another idea, we found the organization simple to navigate as was how they speak to “turning data into meaningful care recommendations.”

Learn How Patients Can Help
Partnerships between doctors, nurses, patients, and caregivers allows for greater engagement.
We say, “Health is not medicine and treatment is not care” perhaps the transformation CMS might be looking to achieve allows for “ownership” that might align with personal responsibility and accountability.
Insurance companies are constantly looking at ways to approach problems that affect the bottom line.
Access to Big Data will transform care models.
Healthcare is no exception as measures migrate towards electronic data collection and submission, a new alignment can emerge.
This is a major focus and the primary reason we created an online presence, watch our Blog page, and social media too.
Community Wellness benefits us all.
Public policy changes will create a “new culture,” one that will include a new era of patient engagement.
AHRQ’s “Evidence NOW” Key Driver Diagram speaks to the “AIM” which is to “Improve heath care quality by increasing the capacity of primary care practices to implement the best clinical evidence.”
Take a look at the Diagram “change strategies” to help you get started, then define what the value of “information” is that can easily absorbed.
Satisfaction involves fulfillment of expectations and meeting the needs with achievement of a new confidence when looking to improve the patient experience. When we involve the consumer from their perspective, we open lines of communication that include taking responsibility for one’s actions.
CAHPS introduced patient satisfaction through HCAHPS which is tied to outcomes within performance thresholds linked to payment. Marketing expert’s used performance data and positive patient response information to promote service lines or create responses to value propositions. Setting yourself apart from your competition through cost savings, quality-of-care, and patient satisfaction which can include features within your patient portal is something to bring to conversations with patients. CAHPS surveys ask patients to report on their experience with a range of services and contribute to “Star Ratings” to learn about these:
- HCAHPS the first survey has the most comparative performance, this hospital survey correlated to the inpatient population has an Adult and Child survey version
- If you are a provider or part of a facility, it’s important to keep your information up-to-date, because patients and families use data to compare, or shop for services in this age of transparency
- CAHPS Clinician & Group Survey (CG-CAHPS) come in two versions and determine the need for improvement activities and evaluate the impact of those efforts
- Patients, relatives, and caregivers are becoming more aware of resources and information to learn more before they select services
CMS Quality of Care Center features “Roadmaps” and Resources that speak to multiple Quality initiatives.
Are you aware of ways to help patients and families? Often times a simple mention of “what to expect” related to care they will receive or inclusion of a website, such as the one below on your patient portal adds to your value
Mental Health and Substance use disorders are an area that has been impacted by the Covid-19 pandemic. The Substance Abuse and Mental Health Services Administration (SAMHSA) has an easy to navigate training site. Are you a Practitioner in need of training? Learn more about:
The Providers Clinical Support System (PCSS) is a national training and clinical mentoring project developed in response to the prescription opioid misuse epidemic and the availability of pharmacotherapies to treat opioid use disorder. PCSS trains health professionals to provide effective, evidence-based, medication-assisted treatments to patients with opioid use disorder in primary care, psychiatric care, substance use disorder treatment, and pain management settings.
Here’s how we are guiding our consumer and caregiver members too
We recognize the value of your feedback as we further develop innovative approaches through various methodologies using both human intelligence and SMART (Self-Monitoring Analysis and Reporting Technology) devices. SMART technology, although the code is written and programmed by human forces uses artificial intelligence, machine learning, and big data analysis to provide cognitive awareness to objects that were in the past considered inanimate (nonliving).
We mention this as we are now moving into a telehealth reality where body part terms are commonly extended to characterize the “anatomy” of inanimate objects.The futuristic state has new treatment paradigms, and the ordinary consumer will be expected to fully engage. In a recent collaborative conversation (2021) mention was made that the “average consumer isn’t generally informed enough to be a part of the conversation” and your staff has an opportunity to educate and engage during all the “touch points” of care delivery. Moving forward
As you navigate this page, we will create sections that address tangible resources such as links specifically to healthcare and wellness from both government mandates and regulatory measures, wellness from environmental and social factors, and how concepts of care will be addressed that allows you to be prepared to “sit at the table” and be a voice for others. Our intention is in providing information only to show what you are not hearing on the local news stations that might be important to take a look at and think about. Have you thought about what or how you want to access care or consider the type of care available? We’re looking for innovative concepts, especially as it relates to what healthcare providers are being tasked with in the future.
In a recent collaborative conversation (2021) mention was made that the “average consumer isn’t generally informed enough to be a part of the conversation” That is an area where we will share our latest findings, concepts, insights and recent work. Your membership with us is specifically focused on “Wellness YOUR Way! We will speak to both barriers and constraints as well as successful approach’s towards Intentional Living, discovering a new learning process to gain in-depth knowledge necessary to finding your voice as a patient or being the voice for someone you care for. Our Blog page will address concepts that are within a process the government is considering and asking for feedback on or related to innovative methods from an approach or mention from social media. Many of our links that guide you to a government site and we have mentioned on the membership pages the following:
Note: Works of the U.S. Government are in the public domain and you don’t need permission to reuse them, but an attribution to the agency as the source is appreciated. Your materials, however, shouldn’t give the false impression that the government’s endorsing your commercial products or services. See 42 U.S.C 1320b-10.
Our intention is to organize the resources and tools into a “one stop shop” online resources methodology as well as provide background on what and why healthcare is changing and options for you to become engaged.
As you navigate this page, we have created and will continue to add sections based off of member feedback, that address tangible resources such as links specifically to healthcare and wellness from both government mandates or regulatory measures, wellness from environmental and social factors, and how concepts of care will be addressed that allows you to be prepared to “sit at the table” and become a voice for yourself and others.
Our intention is in providing information only, not share our opinions as well as to educate you as to what is not discussed on the local news stations or other outlets. This information is both important to think about but to contemplate how the information relates to you or your loved ones.
Have you thought about what or how you want to access care or consider the type of care available? We are looking for innovative concepts, especially as it relates to what healthcare providers are being tasked with in the future. Sharing your experience or what and how a process can be improved aligns with what we call, the “patient voice.”
When we speak to the complexity of a human being often how we care for ourselves is closely related to what we know. Often, we aren’t sure of a possible solution as we aren’t aware of the questions we need to consider. There is a term for this, “you don’t know, what you don’t know, therefore aren’t sure what question to ask.” In healthcare we use a term, “continuum of care” but what does that mean to the average individual from a body, mind and soul point of view?
Additionally, with the overabundance of information on the web; how can the average consumer understand which is the best site? The Affordable Care Act (ACA), enacted in 2010, dramatically changed the U.S. health care landscape. CMS.gov, a federal government website managed and paid for by the U.S. Centers for Medicare & Medicaid Services (CMS) is tasked with keeping the country informed. If you have been a consumer of healthcare services or working in a healthcare facility for over ten years, you are well aware of how advances in technology have greatly changed how you have access to care, medications, medical services, and devices. Surveys are conducted that are mandated and include several pathways and perspectives of care. The Agency for Healthcare Research and Quality (AHRQ) is the lead federal agency charged with improving the safety and quality of America’s health care system. AHRQ develops the knowledge, tools, and data needed to improve the healthcare system and help Americans, health care professionals, and policymakers make informed health decisions. AHRQ has a Leadership Video Series that speaks to:
- Promoting Research and Practice Improvement
- Improving Health Care Practice – working to improve the quality of care patients receive
- Making Health Care Safer – moving toward a safer health care system
The nicely organized AHRQ News Now, listed by calendar order with most recent on top, transparently covers a variety of topics. One directly related to the current pandemic, as we were thrust into Telemedicine with Covid-19, is a part of AHRQ’s National Advisory Council which provides advise and recommendations. One of the articles on “Expanding Telemedicine in the Age of COVID-19” has a link where you can sign up to receive their blog post directly to your in-box.

Whenever you receive services you might get a call from a survey company that is reporting results to the government on behalf of the facility or provider you visited on a specific day or point in time. The Consumer Assessment of Healthcare Providers & Systems (CAHPS) which were first launched by AHRQ in October of 1995 in response to concerns about the lack of good information about the quality of health plans from the enrollees’ perspective. There are multiple CAHPS surveys, poor survey results could result in facilities forfeiting reimbursements. Terms that are important to understand include pay-for-performance (P4P) and Value-Based-Purchasing where you can better understand the pros and cons of performance in healthcare. Let’s look at an example:
If you are a caregiver (family or friend) for a loved one, and dealing with “end of life” there is a survey designed especially for you, a CAHPS Hospice Survey. This national survey of family members or friends who cared for a patient wo died while under hospice care is conducted monthly. The 47-question survey covers topic of interest and is published as a part of Care Compare on the Medicare website. When developing your patient voice, this site can be a good tool for you to use. Look at the table that speaks to the eight measures. On the left side is the “Measure Name” header, and on the right side under the “Questions from the Survey” header you will notice bulleted items that address the types of care that we at Purposeful Concepts references as Body, Mind and Soul which encompasses the “whole person” not just a body part, chart or room number, or case description. The respect one has for a human life must reach beyond just meeting the basic needs. Each of the bullets speaks to a task or “workflow” involved in the care and communication received. When reviewing the caregiver experience, your perception of care is what is collected and reported and is typically handles through a third-party vendor. You will notice under the table there is mention of “Participation Requirements for Hospices” which is important to realize in ALL CAHPS surveys, responses are aligned with reimbursement or the annual payment update (APU) which addresses if full payment from Medicare will be received.
For those not familiar with healthcare terms or want to better understand we can help.
Often language and terms that are used in healthcare can be a barrier to understanding what the next steps look like. When patients and families are asked, do you have any questions, a common response is no. Barriers arise outside the clinical setting or during a Telehealth visit that relate to the process or treatment that needs to be navigated. CMS provides an extensive glossary of over 1000 terms here. If you look to the right side on the page, you will see a link for Acronyms that you can select which provides over 4400 terms. Please reach out if you experience difficulty in understanding the CMS language within federal government benefits, services, or want to send feedback. Speak-Up, your voice is important moving forward.
How do you know?
How do you know if you- are getting the care you deserve? How are you accountable to improve one area of your life, or to share with your loved one related to prevention. How can you limit risk?
Now that you understand the importance of YOUR voice in care and want to better understand how CMS is committed to supporting clinicians and other providers take a look the data collected. Moving forward, electronic health records will be configured to send and receive more and more information. This information wis designed with improvement in mind and you can opt into specific measures that we will make you aware of.
CMS.gov sites are constantly updated to reflect resources and tools for all stakeholders and provides multiple years of comparison on quality of care. Here’s a few service lines you might be interested in:
Need to understand technology and strategy? Learn how to:
- Access your health information necessary to have in an emergent situation
- Use your health data understand how to share your health record, use an app to manage information and more
- Know your Privacy and Security rights and your responsibility to protect your information
- Learn where to find treatment, programs, and multiple 24/7 help lines
- Find Public Messages for concepts to reduce the impact of mental health issues and substance abuse
Let’s think about hospitals now
Did you know over seventy-five percent of the hospitals are recognized as charitable organizations; hospitals must submit IRS Form 990 Schedule H annually to demonstrate their community benefit expenditures and maintain their 501c3 designations. A community health assessment (sometimes called a CHA), also known as community health needs assessment (CHNA), refers to a state, tribal, local, or territorial health assessment that identifies key health needs and issues through systematic, comprehensive data collection and analysis. The CHNA is a systematic process involving the community to identify and analyze community health needs. The process provides a way for community organizations to partner and prioritize health needs, and to plan and act upon the prioritized unmet needs within specific communities. Learn more about the Affordable Care Act (ACA)
CMS is transparent in their reporting and allows users to navigate outcomes data. Keep in mind, some data has a “lag” or “look back” and may not reflect new process improvement measures that are underway. We’ll explain this is further detail through our blog page.
Hospital Compare for over 4000 facilities and a multitude of measures
HCAHPS the hospital version of the survey, this was the first survey that was implemented
Inpatient Rehabilitation Facilities
Long-term Care Hospitals make sure to review the Announcements area
Nursing Homes including Rehab Services as of October 2020 measures are now reported publicly

Two newer services CMS now offers are related to costs and suppliers.
Costs for visits to providers when planning an outpatient procedure are easily navigated through CMS tools. Datasets extracted from these datasets allow you to compare, across specialties and zip codes, minimum, maximum and mode pricing of Medicare-certified suppliers nationwide. Datasets are available for office visits related to 80 physician types including Cardiac Surgery, Pain Management, Pulmonary Disease, Radiation Oncology, Geriatric Medicine, Dermatology, Endocrinology to name a few types and are found by zip code for new and established patients.
A Supplier Directory can be found here too
Are you looking for Chronic Illness Resources? This is an area we would like for you to suggest other additions. We’re starting with:
Allergy-Asthma-Immunology – The Virtual Allergist tool visit
Manage your health and view the pollen count in your area
The National Quality Forum is known for Driving measurable health improvements together to address the care that is needed for people and communities.
The National Quality Forum (NQF) works with members of the healthcare community to drive measurable health improvements together. NQF is a not-for-profit, membership-based organization that gives all healthcare stakeholders a voice in advancing quality measures and improvement strategies that lead to better outcomes and greater value
You can find materials and information transparently to those with access to the internet. The issues they address are available; here are some top areas where consumers/caregivers can learn more and/or get involved.
Here is just one example that may be of interest, what others would you like to see if they are underway?
Maternal Morbidity and Mortality: When we speak to environmental factors that contribute to the biology of a person, we learn from this site that severe maternal morbidity affects more than 60,000 women annually across the United States with rising trends over the last two decades.
Educational materials, past meeting agendas, transcripts and reports are available too.

Here’s some concept examples:
- Is the information conceptual (ideas that simplify)
- Am I declaring something? Qualitative
- Is the information data-driven (statistics to inform or enlighten)
- AM I exploring something? Quantitative
When we are caring for our bodies often times this is where clinical healthcare services are aligned, think of what you typically are provided through health insurance coverage, a multitude of care options are aligned with “regulatory measures” that encompass metrics around quality, safety and patient experience (satisfaction). This area is where consumers will be called to “sit at the table” and share their thoughts in a concise and professional manner. We will be walking you through the specifics as they emerge in 2021 and beyond. There is a public comment period on policy before it takes effect, we will draft sample responses options to help you gather your thoughts for submission. Be the VOICE in what Patient and Family Centered Care can become and review some free resources.
Are you a specialist? Did you know…
